Coronary artery disease (CAD) is the leading cause of death in the United States, often remaining undetected until a heart attack occurs. While effective treatments for prevention do exist, they are frequently underused—mainly because individuals are unaware of their personal risk levels. A recent breakthrough published in Nature Medicine on April 16, 2025, by researchers at the Scripps Research Translational Institute offers a new solution: a personalized predictive model that significantly improves the accuracy of CAD risk assessment.
Unlike traditional clinical tools that rely heavily on age and general health indicators, this new machine learning–based model considers a wide range of personal factors. These include genetic predispositions, lifestyle choices, family medical history, mental health conditions, sleep duration, blood biomarkers, and more. By analyzing data from the UK Biobank involving over half a million individuals, the research team initially started with about 2,000 possible risk factors and refined the model down to 53 key predictors of CAD.
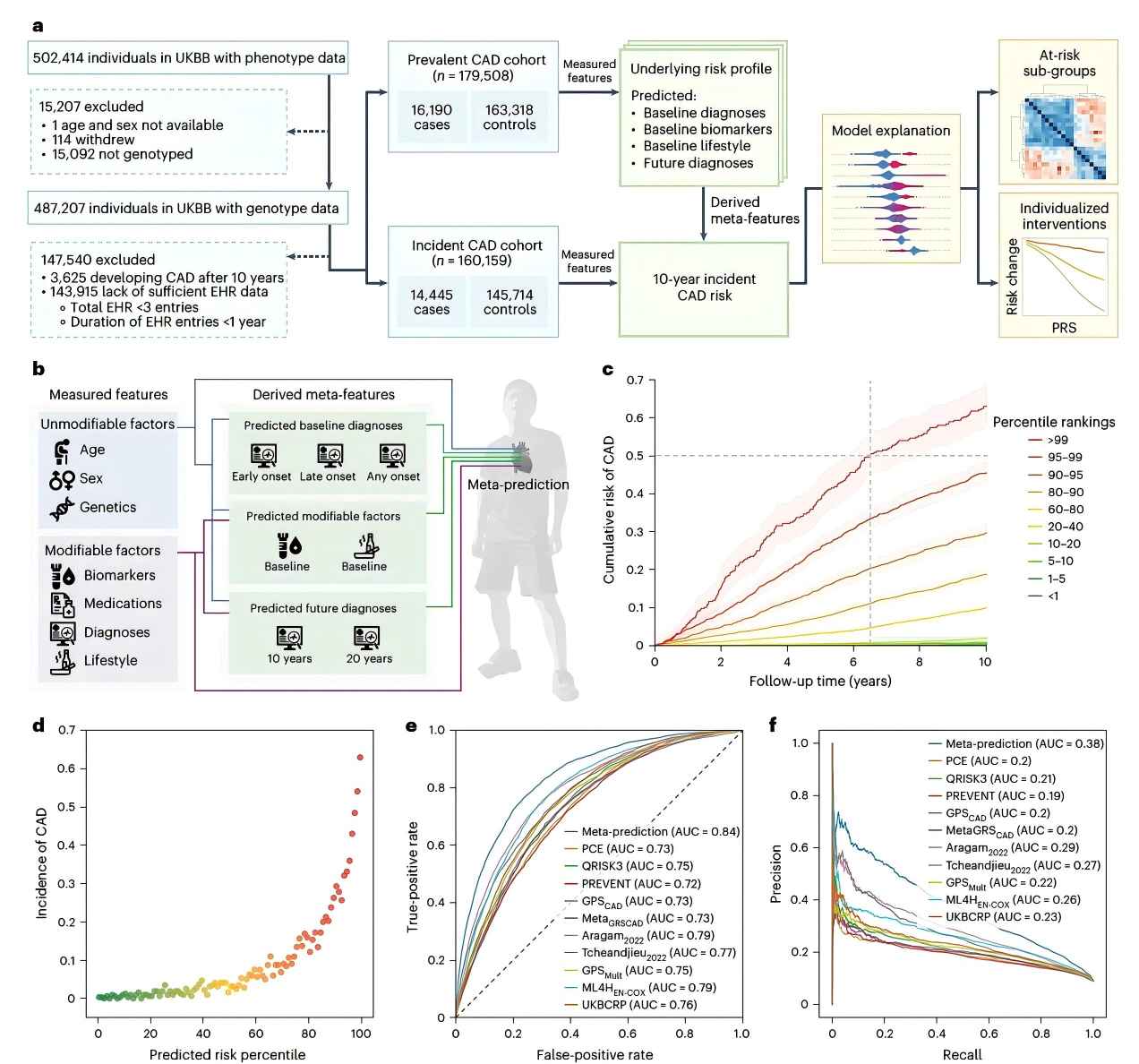
The results were remarkable. Over a 10-year follow-up, nearly 63% of people categorized by the model as "high risk" eventually developed CAD. In contrast, only 0.3% of those in the "low risk" group did. Notably, the new model improved risk classification for approximately one in four individuals, outperforming conventional methods and reducing false positives and false reassurance. Particularly impressive was its ability to detect high-risk individuals who would traditionally be considered low-risk due to their age or gender—groups such as younger adults and women.
One of the strongest insights from the study was the role of genetics in CAD development. The model found that people with a high genetic predisposition to traits like high cholesterol, high blood pressure, or type 2 diabetes were also at greater risk of developing CAD. These insights allow for highly targeted preventive strategies, ranging from lifestyle modifications to early medical interventions.
Importantly, the model's accuracy held across diverse populations. When tested on data from the U.S. National Institutes of Health's All of Us program—which includes individuals of European, African, and Hispanic ancestry—the model demonstrated consistent predictive performance, highlighting its potential for global clinical use.
Moving forward, the research team plans to launch a long-term clinical trial to test whether informing individuals of their personal CAD risk will encourage behavioral change and reduce disease incidence. According to the study's authors, the ultimate goal is to empower patients with precise information so they can make informed health decisions long before symptoms appear.
This "meta-prediction" approach represents a major leap in preventive cardiology. By integrating advanced data science with personalized medicine, it opens the door to a future where heart disease is not only treatable—but preventable.
Read More:Nature Medicine






Post comments