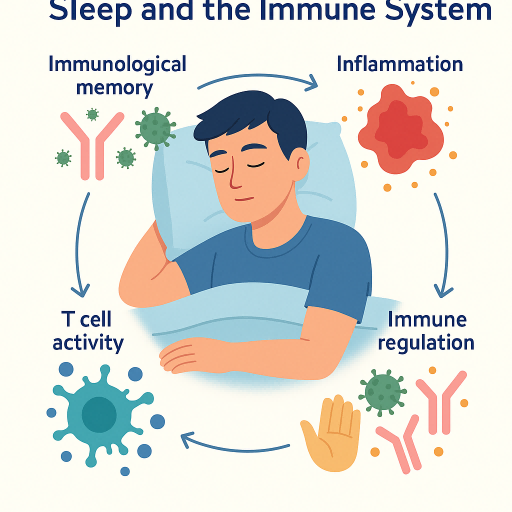
Introduction: Why Sleep and Immunity Matter
Sleep is a fundamental biological process essential not only for cognitive and physical restoration but also for the optimal functioning of the immune system. Far from being passive rest, sleep serves as a critical period of immune regulation, during which the body fine-tunes its defense mechanisms against pathogens. The relationship between sleep and immunity is bidirectional: while adequate sleep supports both innate and adaptive immune responses—enhancing cytokine production, immune cell trafficking, and immunological memory—immune activation itself can alter sleep patterns.1,2
Mounting evidence indicates that sleep deprivation disrupts these processes, increasing systemic inflammation, elevating pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), and impairing hematopoietic stem cell function. These alterations compromise immune surveillance and host defense, heightening vulnerability to infections. In this context, sleep emerges as a dynamic and active state of immune calibration and preparedness, integral to maintaining health and resisting disease.3
Sleep Architecture and Immune Modulation
Sleep architecture—comprising non-rapid eye movement (NREM) and rapid eye movement (REM) stages—plays a central role in immunological homeostasis. Among these, slow-wave sleep (SWS), the deepest phase of NREM, is particularly important for immune restoration. During SWS, production of pro-inflammatory cytokines such as IL-1 and TNF-α is elevated4. These cytokines not only regulate sleep intensity but also promote adaptive immune responses and the consolidation of immunological memory.
In contrast, REM sleep is often suppressed during active immune responses, suggesting that sleep stages may be selectively modulated based on immunological demand. Circadian rhythms further synchronize immune activity, with melatonin—secreted during the night—playing a key immunoregulatory role. Melatonin enhances antioxidant defenses, reduces oxidative stress, and modulates inflammatory signaling pathways.
Disruption of normal sleep architecture or circadian timing, such as from shift work or chronic sleep loss, undermines these immunological processes. The result is increased susceptibility to infection, impaired vaccination response, and heightened risk of chronic inflammatory disease. Thus, sleep functions as an essential biological mechanism for maintaining immune balance and resilience.5,6,7
The Immunological Cost of Sleep Deprivation
Extensive experimental research confirms that even short-term sleep deprivation has immediate and measurable effects on immune competence. Notably, natural killer (NK) cell activity—a frontline defense against virally infected and malignant cells—declines significantly after a single night of sleep restriction8. Concurrently, levels of pro-inflammatory mediators such as IL-6 and TNF-α rise, promoting a systemic inflammatory milieu9.
Moreover, elevated cortisol levels associated with poor sleep further suppress immune function by inhibiting lymphocyte proliferation and activity. These physiological changes translate into clinically relevant consequences: slower wound healing, increased susceptibility to respiratory infections, poorer COVID-19 outcomes, and reduced vaccine efficacy, including diminished antibody responses following influenza and hepatitis A immunizations10.
In sum, inadequate sleep imposes a cumulative immunological burden, diminishing host defense and amplifying the risk of both infectious and non-communicable diseases. This highlights the public health importance of sleep promotion strategies in both clinical and community settings.
Sleep as a Mediator in Chronic Inflammatory Disease
Chronic sleep disturbance has been identified as a significant contributor to low-grade systemic inflammation, a common pathophysiological thread across numerous chronic conditions—including cardiovascular disease, type 2 diabetes, and cancer. Mechanistically, sleep deprivation induces upregulation of pro-inflammatory biomarkers such as IL-6 and C-reactive protein (CRP), and activates nuclear factor kappa B (NF-κB)—a master regulator of inflammatory gene expression11.
Experimental studies have shown that even partial sleep restriction can lead to increased transcriptional activity of inflammatory genes and elevated circulating cytokine levels. Over time, this persistent inflammatory activation accelerates biological aging of the immune system, a process referred to as “inflammaging.” This state not only undermines immune competence but also increases vulnerability to age-related illnesses, including neurodegenerative disorders and atherosclerosis.12
By amplifying inflammatory signaling and impairing immune resilience, sleep loss serves as both a precipitating and perpetuating factor in chronic disease. Recognizing sleep health as a modifiable risk factor offers clinicians a tangible intervention point for the prevention and management of long-term inflammatory conditions.
References:
Sleep Foundation. How Sleep Affects Immunity. 2023.
Besedovsky L, Lange T, Born J. Sleep and Immune Function. Physiol Rev. 2021;101(3):1187-1216. [PMCID: PMC3256323]
Brouwers TMJ, et al. The effect of sleep and shift work on the primary immune response: implications for health and disease. J Sleep Res. 2024;33(1):e13789. [PMID: 39658344]
Lange T, et al. The Sleep-Immune Crosstalk in Health and Disease. Front Immunol.2024;15:115678.
Besedovsky L, et al. Sleep and Immune Function. Physiol Rev. 2021;101(3):1187-1216.
Human sleep and immunity: The role of circadian patterns. Front Neurosci. 2024;18:
Schilling C, et al. Sleep and Immune System Crosstalk: Implications for Inflammatory Homeostasis. J Clin Med. 2024;13(9):4567.
Tang N, Zeng Y, He G, Chen S. Interference between immune cells and insomnia: a bibliometric analysis from 2000 to 2023. Front Neurol. 2025 Mar 26;16:1486548. doi: 10.3389/fneur.2025.1486548. PMID: 40206297; PMCID: PMC11978667.
Ferreira RCM, Ruiz FS, de Mello MT. Human sleep and immunity: The role of circadian patterns. Handb Clin Neurol. 2025;206:93-103. doi: 10.1016/B978-0-323-90918-1.00003-4. PMID: 39864935.
Garbarino, S., Lanteri, P., Bragazzi, N.L. et al. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol 4, 1304 (2021). https://doi.org/10.1038/s42003-021-02825-4
Irwin MR. Sleep disruption induces activation of inflammation and heightens risk for infectious disease: Role of impairments in thermoregulation and elevated ambient temperature. Temperature (Austin). 2022 Aug 21;10(2):198-234. doi: 10.1080/23328940.2022.2109932. PMID: 37332305; PMCID: PMC10274531.
Ballesio A. Inflammatory hypotheses of sleep disturbance - depression link: Update and research agenda. Brain Behav Immun Health. 2023 Jun 22;31:100647. doi: 10.1016/j.bbih.2023.100647. PMID: 37408788; PMCID: PMC10319168.







Post comments