Introduction: Preeclampsia and the Need for Innovation
Preeclampsia is a leading cause of maternal and fetal morbidity and mortality, affecting 2–8% of pregnancies globally. Each year, it accounts for approximately 46,000 maternal and over 500,000 fetal deaths, disproportionately burdening low-resource settings and vulnerable populations. Despite significant advances in obstetric care, current diagnostic methods—centered on elevated blood pressure, proteinuria, and a limited set of biomarkers—often detect the condition only after clinical symptoms have emerged. By then, opportunities for timely intervention may already be lost, increasing the risk of complications such as eclampsia, HELLP syndrome, and future cardiovascular disease in both mother and child.
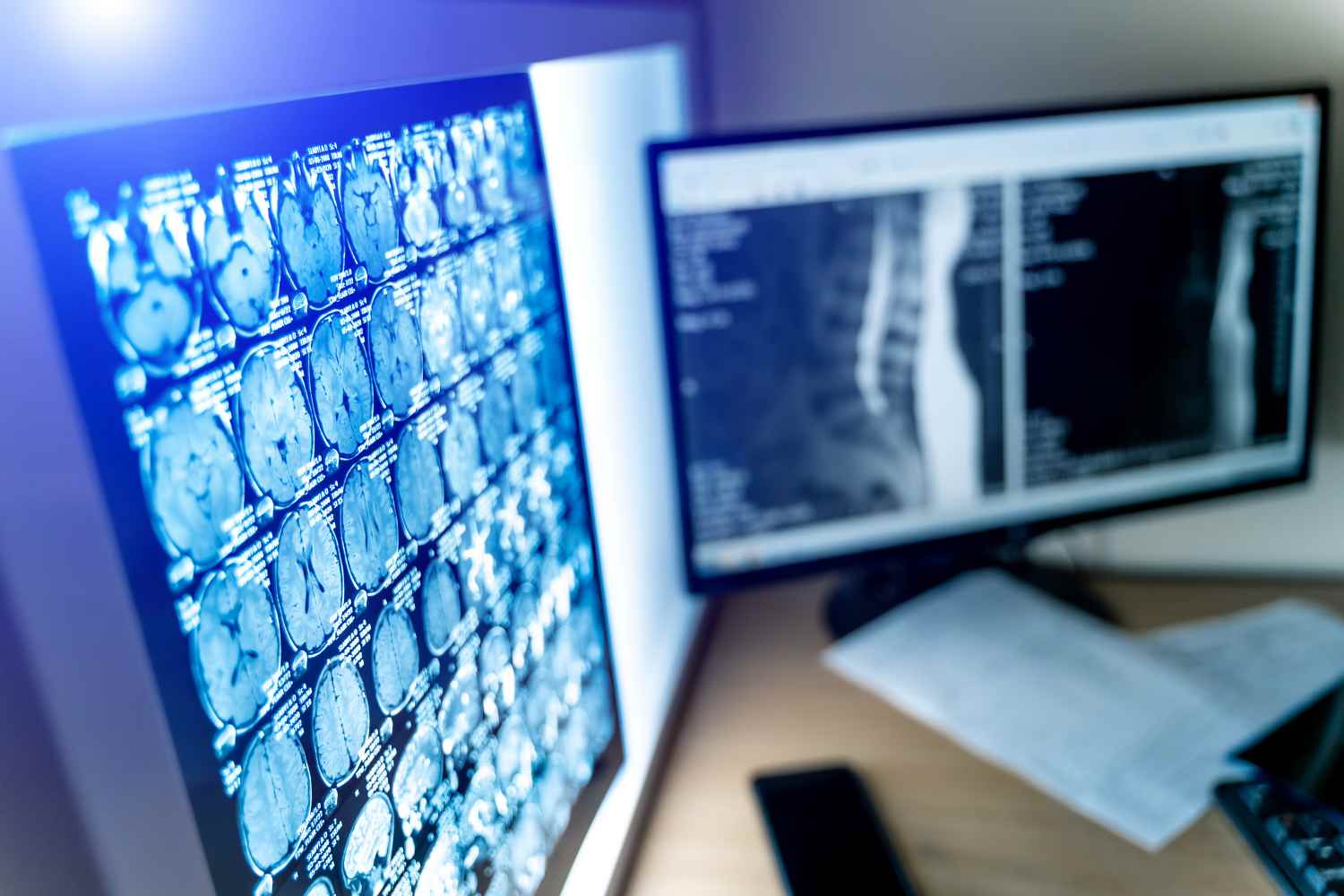
The urgency for a scalable, non-invasive method that can identify preeclampsia early in gestation is evident. One promising avenue lies in an often-overlooked anatomical region: the retina. Retinal vessels offer a non-invasive and accessible window into systemic microvascular health, and recent advances in artificial intelligence (AI) have enabled high-precision analysis of subtle vascular changes through ocular imaging. This convergence of AI-powered diagnostics and retinal imaging marks a turning point in maternal health, offering new possibilities for early detection, personalized risk stratification, and proactive management of preeclampsia—potentially reshaping prenatal care on a global scale.
The Retina: A Microvascular Mirror of Maternal Health
The retina is uniquely suited to reflect maternal vascular status due to its embryological and physiological similarities to the placental vasculature. Both systems rely on delicate endothelial linings and extensive microcirculatory networks, which are particularly vulnerable to systemic vascular dysfunction—hallmarks of preeclampsia. In preeclamptic pregnancies, retinal vessels commonly exhibit signs of arteriolar narrowing, increased tortuosity, and altered fractal geometry. These retinal manifestations mirror placental pathology, including reduced perfusion and endothelial damage, supporting the notion that retinal imaging can serve as a proxy for maternal vascular health.
Non-invasive modalities such as fundus photography and optical coherence tomography angiography (OCTA) allow clinicians to visualize and quantify retinal vascular parameters, including vessel caliber, branching patterns, and tortuosity, with high resolution and minimal risk. Evidence is accumulating that these metrics are altered even before the clinical onset of preeclampsia. Studies have identified reductions in central retinal arteriolar and venular equivalents early in pregnancy among women who later develop the condition. In some cases, microvascular remodeling persists well into the postpartum period, further supporting the retina’s role as a surrogate biomarker of systemic vascular pathology.
Moreover, recent pilot studies have demonstrated the utility of advanced AI tools to analyze these retinal images, quantifying subtle changes that may elude traditional examination. Features such as vessel width variability, branching angle asymmetry, and tortuosity indices have been shown to correlate with disease severity and may offer earlier predictive value than conventional clinical indicators. These findings validate the clinical relevance of retinal imaging as a non-invasive, scalable tool for identifying vascular compromise in preeclampsia.
Clinical Implications: Toward Scalable and Equitable Screening
The integration of AI with retinal vascular imaging opens the door to a transformative model of prenatal care—one that is proactive, scalable, and equitable. Traditional approaches to preeclampsia screening rely on repeated clinical visits, laboratory tests, and specialized equipment, all of which are often inaccessible in rural or resource-limited settings. In contrast, portable retinal imaging devices, including smartphone-based fundus cameras, provide a low-cost and user-friendly solution that can be deployed at the point of care, even outside hospital settings.
When paired with AI algorithms capable of analyzing retinal features in real time, these tools can stratify patients by risk level as early as the first trimester. This allows for early intervention strategies, such as enhanced monitoring, lifestyle modifications, or prophylactic therapies, before the clinical onset of disease. The potential for population-level screening—delivered through community health programs or telemedicine platforms—is especially compelling in regions with limited access to obstetric specialists.
Clinical validation of this approach is growing. The PROMPT study demonstrated that AI-assisted retinal image analysis could predict preeclampsia with area under the curve (AUC) values as high as 0.91, while maintaining cost-effectiveness and suitability for integration into routine prenatal care. Other studies have shown that nonmydriatic, AI-interpreted retinal imaging performs well in low-light and field conditions, with promising results in both urban hospitals and remote clinics. Furthermore, research into AI systems that incorporate additional data—such as blood pressure trends or wearable sensor outputs—suggests a future in which retinal imaging is part of a broader, multimodal screening strategy.
By reducing the need for invasive testing and increasing access to high-quality prenatal screening, AI-enhanced retinal imaging has the potential to reshape maternal healthcare delivery. It offers not just a diagnostic tool, but a platform for early detection, personalized risk management, and better maternal-fetal outcomes—aligning with global goals for improving maternal health equity and reducing preventable deaths.
Reference:
1. Maternal mortality - World Health Organization (WHO)
2. Pribadi A, Hidayat D, Sasotya RMS, Aziz MA, Nurdiawan W, Pramatirta AY, Siddiq A, Mose JC, Hidayat YM, Nugrahani AD, Santoso DPJ, Permadi W. Assessing the Impact of the Zero Mother Mortality Preeclampsia Program on Maternal Mortality Rates at a Single Center in Bandung, West Java (2015-2022): A Retrospective Study. Med Sci Monit. 2023 Jul 23;29:e941097. doi: 10.12659/MSM.941097. PMID: 37481698; PMCID: PMC10373510.
3. Karrar SA, Martingano DJ, Hong PL. Preeclampsia. [Updated 2024 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK570611/
4. Australian Institute of Health and Welfare. (2025). Australia's mothers and babies. Retrieved from https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-babies
5. Soma-Pillay P, Pillay R, Wong TY, Makin JD, Pattinson RC. The effect of pre-eclampsia on retinal microvascular caliber at delivery and post-partum. Obstet Med. 2018 Sep;11(3):116-120. doi: 10.1177/1753495X17745727. Epub 2018 Mar 7. PMID: 30214476; PMCID: PMC6134356.
6. Abu Samra K. The eye and visual system in the preeclampsia/eclampsia syndrome: What to expect? Saudi J Ophthalmol. 2013 Jan;27(1):51-3. doi: 10.1016/j.sjopt.2012.04.003. Epub 2012 Apr 23. PMID: 23964188; PMCID: PMC3729391.
7. Wu, Y., Shen, L., Zhao, L. et al. Noninvasive early prediction of preeclampsia in pregnancy using retinal vascular features. npj Digit. Med. 8, 188 (2025). https://doi.org/10.1038/s41746-025-01582-6
8. Zhou T, Gu S, Shao F, Li P, Wu Y, Xiong J, Wang B, Zhou C, Gao P, Hua X. Prediction of preeclampsia from retinal fundus images via deep learning in singleton pregnancies: a prospective cohort study. J Hypertens. 2024 Apr 1;42(4):701-710. doi: 10.1097/HJH.0000000000003658. Epub 2024 Jan 15. PMID: 38230614; PMCID: PMC10906188.
9. Butler L, Gunturkun F, Chinthala L, Karabayir I, Tootooni MS, Bakir-Batu B, Celik T, Akbilgic O and Davis RL (2024) AI-based preeclampsia detection and prediction with electrocardiogram data. Front. Cardiovasc. Med. 11:1360238. doi: 10.3389/fcvm.2024.1360238
10. Bellingeri C, Beneventi F, De Maggio I, Spada C, Smaghi AB, Cortese M, Ligari E, Alpini C, Spinillo A. First trimester preeclampsia screening and risk of placental lesions. Pregnancy Hypertens. 2025 Jul 3;41:101236. doi: 10.1016/j.preghy.2025.101236. Epub ahead of print. PMID: 40614692.
11. Yang Q, Bee YM, Lim CC, Sabanayagam C, Yim-Lui Cheung C, Wong TY, Ting DSW, Lim LL, Li H, He M, Lee AY, Shaw AJ, Keong YK, Wei Tan GS. Use of artificial intelligence with retinal imaging in screening for diabetes-associated complications: systematic review. EClinicalMedicine. 2025 Feb 18;81:103089. doi: 10.1016/j.eclinm.2025.103089. PMID: 40052065; PMCID: PMC11883405.







Post comments